Home > NF2 Facts and Information >
Bilateral Vestibular Hypofunction - Vestibularopothy
Last Updated: 07/15/20
Vestibular Balance Issues
Index
- Vestibulopathy:
Vestibular Schwannomas Damage - Vestibular Rehabilitation Therapy (VRT)
- Basic Balance Recovery Tips
Also See:
People with neurofibromatosis type 2 (NF2) develop walking issues for many reasons.
Most often the walking issue starts as a result of imbalance from tumor growth that results in vestibular nerve damage, which is a branch of cranial nerve 8 that runs from the brainstem to the vestibular system for which provides the inner ear for balance.
The growth of a schwannoma tumor on the vestibular nerve, vestibular schwannomas (VS)/acoustic neuroma (AN) , will result in an individual facing single-sided vestibular system damage and will be the start of a equilibrium issues, bilateral vestibular hypofunction (BVH. BVH is a issue of disequilibrium often accompanied with eye isse of oscillopsia (ocular flutter) that can be treated with vestibulopathy. Single-sided vestibulopathy is vestibular system damage on one side of the head. It results in imbalance issues that an individual can recover from in a few days or a few months.
Bilateral vestibulopathy is vestibular system damage to the vestibular nerve on both sides of the head. "The symptoms typically include imbalance and visual disturbance. The imbalance is worse in the dark or in situations where footing is uncertain while spinning vertigo is unusual. The visual symptoms referred to as "oscillopsia," only occur when the head is moving (J.C., 1952)."[1] Bilateral vestibulopathy results in complete loss of the part of the body that distinguishes motion. With time, a section of the brain will help with adaption to motion, but vestibular rehabilitation therapy (VRT) is necessary.
Without VRT it is easy to develop muscle weakness and over time potentially result in an inability to walk at all.
"Current evidence is in support of VRT for treating patients with a variety of vestibular disorders, both central and peripheral. High-level evidence studies support the use of treatment techniques of adaptation and substitution for gaze stabilization, habituation, balance and gait training, and can with repositioning maneuvers. Recent evidence has also examined and found promising results with technological innovations that are targeted at those with bilateral vestibular hypofunction and insufficient gains with a standard exercise-based program. Nevertheless, factors such as anxiety overlay/depression, a time when beginning therapy, and adherence may have an impact on how a patient will do with his/her VRT program and should be acknowledged." [Burzynski, 2017]
Sometimes balance issue is indirectly from vestibulopathy, like medications that can increase disorientation, other brain tumors, or weak core muscle strength. Talk to your doctor.
1. Vestibulopathy: Vestibular Schwannomas Damage
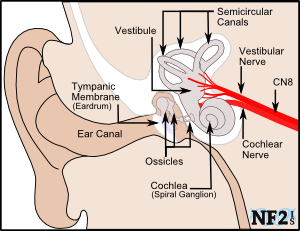 Inner Ear System |
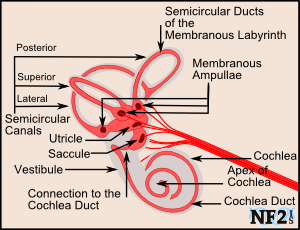 Inner Vestibule |
 Gyroscope: Source Wikipedia |
The most common location for tumors to grow for individuals with NF2 is in the brain along the Vestibular Nerves. The tumors are an overgrowth of a section or sections of the nerve, an overgrowth of the schwann cell. There are two vestibular nerves left and right, one on each side of the brain since there are two cranial nerves for each nerve type, one affecting the left and the other the right side of the body. The Vestibular Nerve is responsible for the function of the vestibular system which is responsible for balance.
Vestibular Schwannoma (VS) that grow on a Vestibular Nerve will typically also damage the cochlear nerve as well. The cochlear nerve is responsible for the function of the cochlea and therefore hearing. Cranial Nerve 8 (CN VIII), the Vestibulocochlear Nerve starts at the brainstem and splits to become the vestibular nerve and the cochlear nerve.
The three semicircular canals of the vestibular system can be best understood by understanding the workings of a gyroscope, used by ships and planes.
Since it can be a slow process from the point one nerve starts to become damaged to the point where both nerves are completely broken, individuals with NF2 tend to adjust better and faster than individuals whose nerves are damaged for other reasons. However; since vision is used to compensate for the loss of these nerves, in bad vision situations like night or if vision issues develop, balance issues will continue to be a problem.
2. Vestibular Rehabilitation Therapy (VRT)
Vestibular rehabilitation therapy (VRT) is very important following vestibular nerve damage. The dizziness, vertigo, balance problems, and other symptoms can lead to unnatural standing and walking methods. This improper compensation can be even harder to correct, lead to worsening of symptoms and often causing headache, muscle tension, and fatigue.
VRT is an exercise program used to treat people of many different ear conditions that result in damaged Vestibular Nerves. Because of the number of people with these issues, people trained to do VRT are not hard to find.
- some balance may be recovered through exercise or balance therapy
- your doctor may be able to refer you to a therapy specialist experienced in balance treatment
- perseverance can help achieve results, but it is important that a medical doctor ensure that any regime is safe for the patient
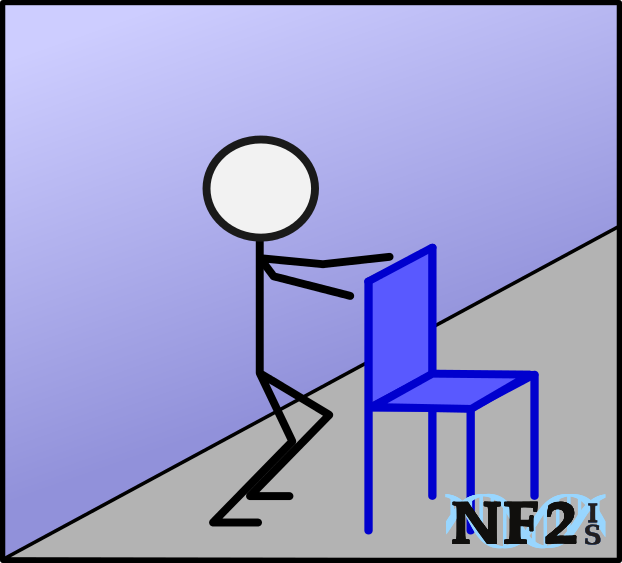
3. Basic Balance Recovery Tips
First attempts at the different movement from vestibular issues for recovery should be done with the presence of another individual. Since the progression of vestibular damage is different for everyone, it is important to get help from a physical therapist. Differences include duration from beginning to complete failure of vestibular system loss bilaterally.
1. Avoiding Medications (Ototoxic) - Strong Prescription Pain Killers
When attempting recovery of balance after vestibular system damage or failure, avoid or discontinue taking prescription strength pain killers as soon as possible. Tylenol #3, Percocet, and Codeine include side effects of lightheaded and dizzy; which makes it difficult to recover from vestibular nerve damage.
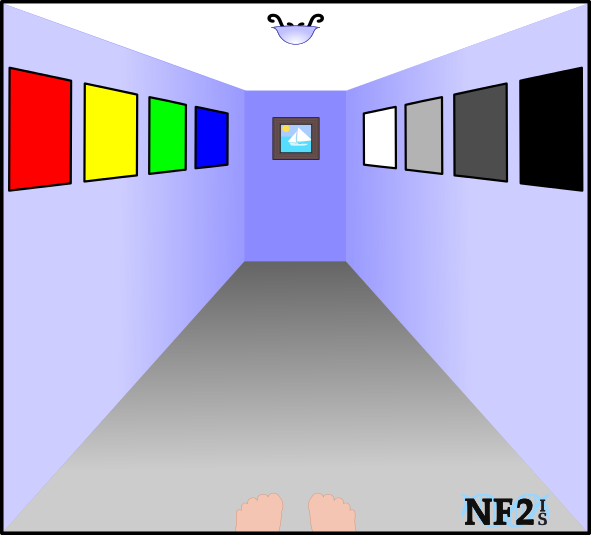
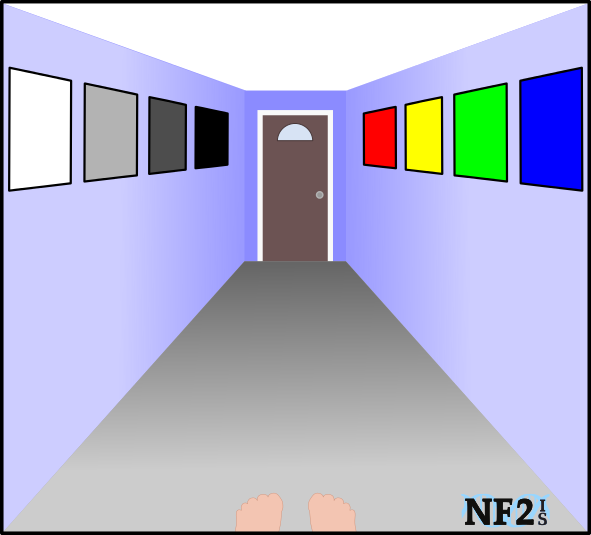
2. Visual Cues and Lighting
Vision for visual cues are necessary for walking stability following vestibular nerve damage. Since vision is needed for stability, it is common to have problems walking at night or in other low or no light situations.
Visual cue examples: 1) Look at a fixed point in the distance to walk towards. 2) Do not look down at your feet on the ground even if vision is blurry. 3) Looking at a streetlight, sign, or other object ahead of you. 4) Look at a picture on a wall. 5) Look ahead at the end of the aisle at the grocery store. 6) look at the face of the person you are walking to meet.
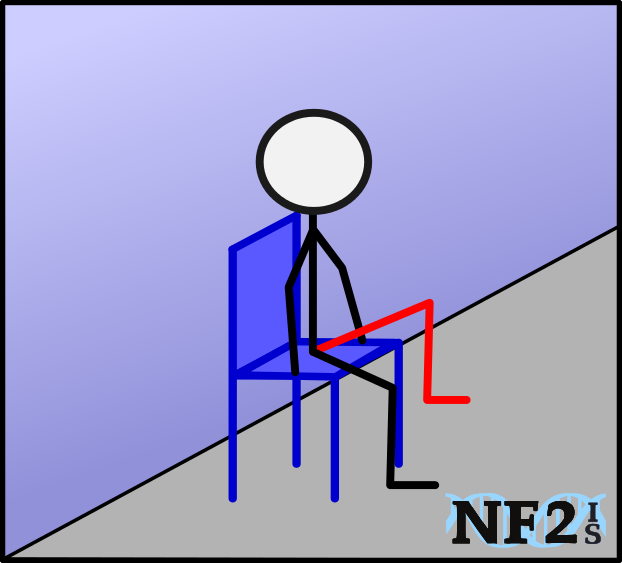
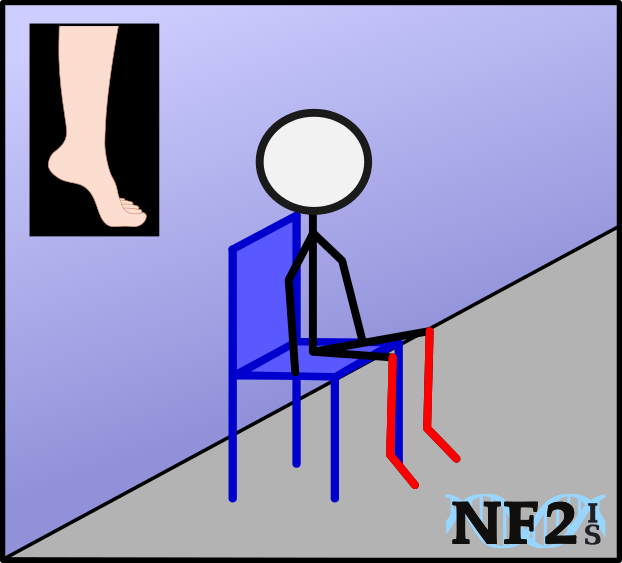
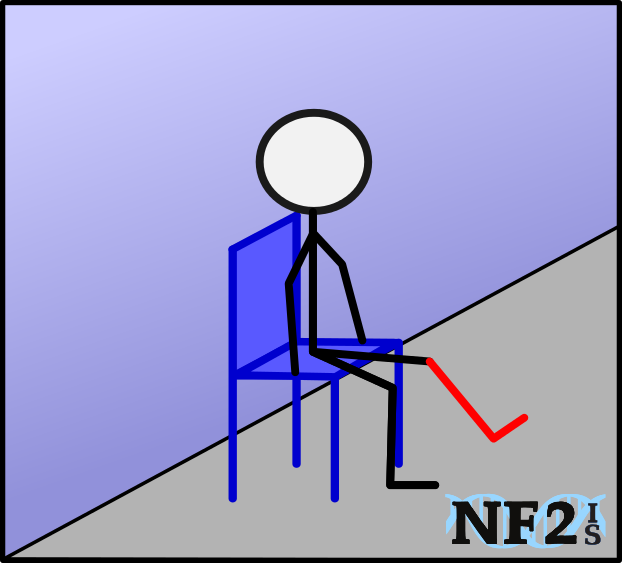
3. Core and Leg Muscles
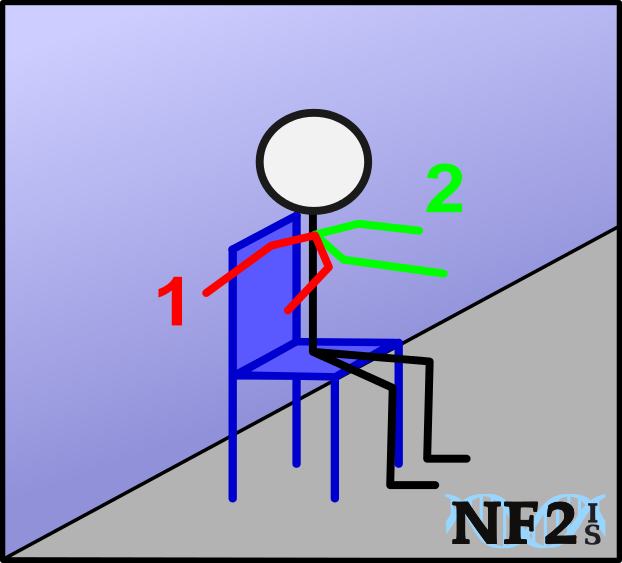
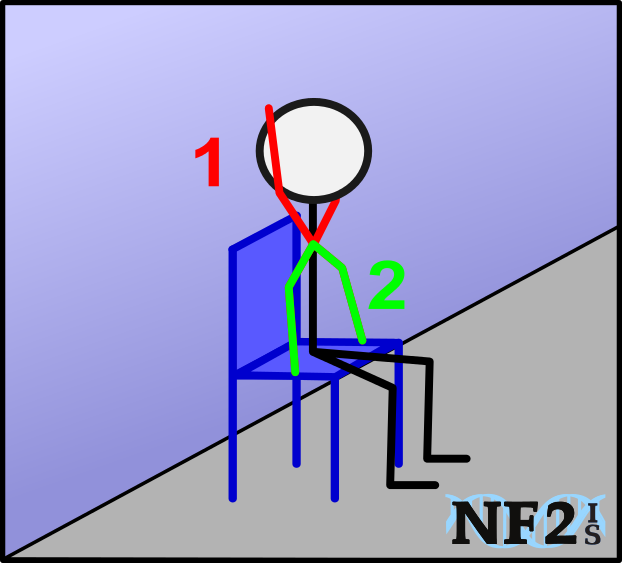
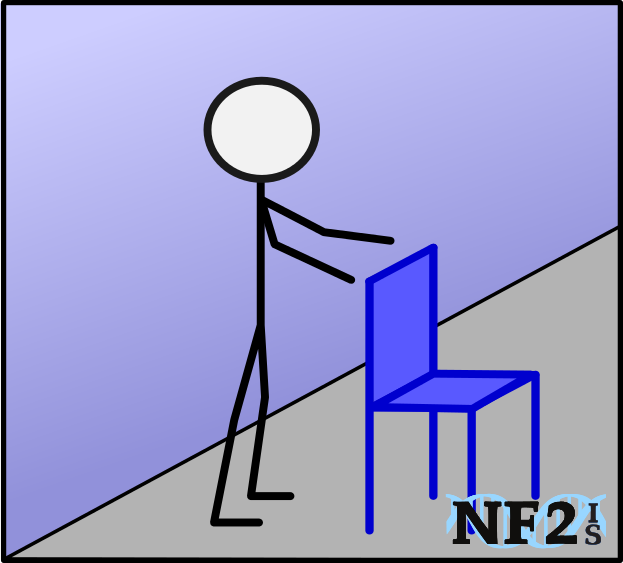
Poor balance quickly results in less overall movement that can result in no muscle strength which will make it difficult to walk again. Find exercise options that can be done; 1) in a seated position, 2) standing with some sort of support like a wall or chair, or 3) while lying down.
4. Flat Floor
Medication, visual cues and muscle strength will help when walking on flat and even surfaces, but the practice of walking backward or on uneven terrain (like grass) can help with fall prevention. - Methods to build balance should not be done while alone.
5. Posture
Remember to stand with your back straight, chest out, and head up looking forward as far as possible. Vestibular system issues cause an automatic response that include slouched shoulders and hands held forward to grasp something for stability: if continued, these balance compensation attempts will cause spine issues.
6. Be Prepared - Know Yourself
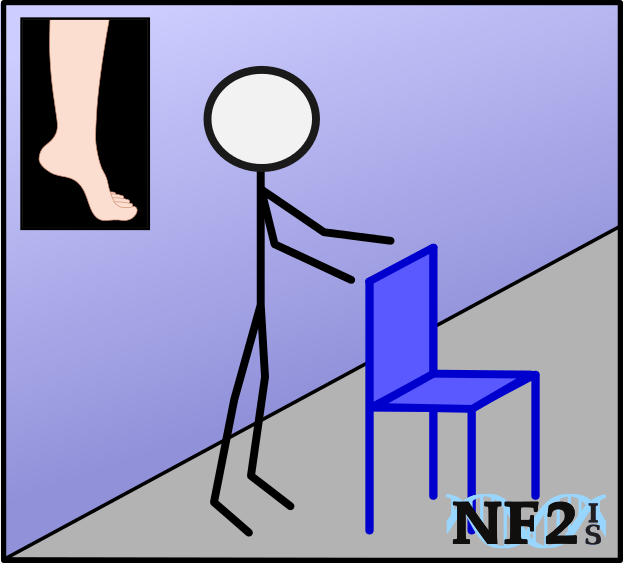
Speak to either a physical therapist, about the best shoes to wear for better balance. Learn how to use a cane for stability, or consider a balance service dog.
* Note: Some Pain Killers including; 1) Codeine, 2) Percocet, and 3) Tylenol #3, can cause Lightheadedness and Dizziness. Taking these things can make walking after Vestibular Nerve damage even more difficult.
4. Source
-
"Bilateral Vestibulopathy." Dizziness and Balance.com (March 24, 2018)
https://www.dizziness-and-balance.com/disorders/bilat/bilat.html - Acoustic Neuroma Association. https://www.anausa.org/
- VEDA. Vestibular Disorder Association. Vestibular Rehabilitation Therapy (VRT). "What Is Vestibular Rehabilitation Therapy? ?" https://vestibular.org/understanding-vestibular-disorder/treatment/treatment-detail-page
-
"The Differential Diagnosis of Meniere's Disease and Vestibular Migraine" Department of Communication Disorders (2017)
https://ir.canterbury.ac.nz/bitstream/handle/10092/13438/MAud%20thesis%20-%20Jon%20Osborne.pdf?sequence=1 -
Burzynski, Joanna. "Vestibular Rehabilitation: Review of Indications, Treatments, Advances, and Limitations."
Department of Otolaryngology, Toronto General Hospital University Health Network (UHN) Toronto, Canada
Current Otorhinolaryngology Reports. pp 1-7 (July 2017)
https://link.springer.com/article/10.1007/s40136-017-0157-1 -
Bisht, Manisha, and S. S. Bist. "Ototoxicity: the hidden menace." Indian Journal of Otolaryngology and Head & Neck Surgery 63.3 (2011):
255-259.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3138949/ -
Emmanouil, Beatrice, et al. "First report of the efficacy of vestibular rehabilitation in improving function in patients with Neurofibromatosis type 2: an observational cohort study in a clinical setting."
Disability and rehabilitation (2018): 1-7.
Source: https://www.tandfonline.com/doi/abs/10.1080/09638288.2018.1442505 | DOI: https://doi.org/10.1073/pnas.1719966115 -
Black, F. Owen. "Acquired bilateral peripheral vestibulopathy." Handbook of Clinical Neurophysiology 9 (2010): 333-352.
Source: https://www.sciencedirect.com/science/article/pii/S156742311009026X | DOI: https://doi.org/10.1016/S1567-4231(10)09026-X - ABD Mideast "Rotundum Rotary Positioning Chair." (Link Added: July 2020) http://www.abd-mideast.com/Rotundum.html


 |Google Play
|Google Play