Home > Treatment Management >
Radiation-based Treatments
Radiosurgery

Index
- Introduction
- Ionizing Radiation
- Non-ionizing Radiation
- Brain Treatment Risks
- Advantages
- Radiosurgery Delivery Methods
- Questions to Ask
- Sources
1. Introduction
The condition neurofibromatosis type 2 (NF2) leaves patients with tumor growth starting at birth, with risk of more in their lifetime. However; the tumors typically grow slow enough, issues from tumors may not develop until teen years or after. Each individual is different.
Treatment for tumor management include; 1) radiosurgery of some form, 2) surgical removal of tumors, resection, 3) tumor-drug treatment, and 4) watch and wait.
Radiosurgery is surgery using precisely targeted radiation to destroy tissue without cutting. [merriam-webster dictionary] Radiosurgery options include gamma knife due to its precision of treatment over CyberKnife. Treatment of proton therapy (proton beam/LINAC) is slowly becoming more available and holds better holds better accuracy than gamma knife.
It is important to understand the pros, cons and have questions surrounding these treatments if considering radiation therapy with a doctor. While radiation treatment may be a good choice to take care of an immediate tumor problem, it can result in problems weeks, months or even years later. (Cancer Connect, 2014)
2. Radiation Brain Tumor Risks
Some of the concerns of radiation therapy are related to changes in the tumor.
1. Effectiveness
The success or failure of treatment is unknown until changes can be detected. Treatment is deemed a success if the tumor stops growing or shrinks and a failure if it continues to grow. These changes can take up to six months to see on an MRI. Also radiation can result in initial tumor swelling before shrinking or stabilizing. Even if a tumor might eventually shrink after treatment, there could be potentially harmful consequences of swelling depending on tumor shape and location.
There can be further complications even when tumors to shrink, the shrinkage may only last for a period of years and if the tumor begins to grow, but radiated tumors have a chance of require follow up treatment. Radiation treatments change the consistency of the tumor mass making subsequent surgery more complicated. It may also result in more extensive nerve damage if surgical removal is required.
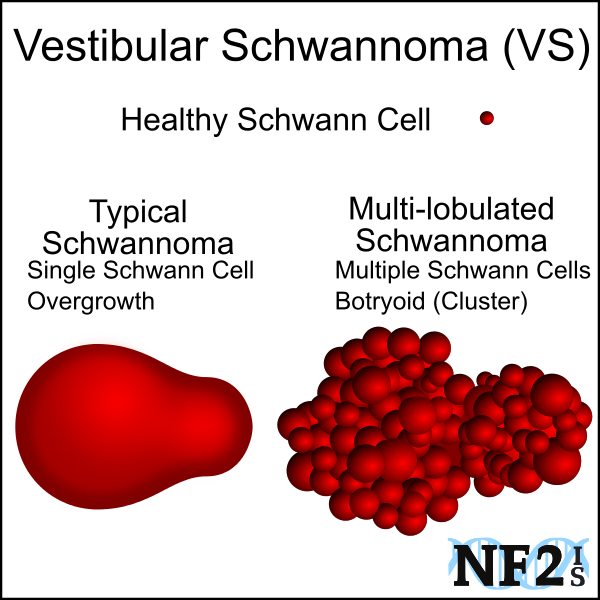
Since NF2 vestibular schwannoma, acoustic neuroma tumors are masses consisting of small schwannoma on more than one nerve fiber of cranial nerve 8 and sometimes 7, during treatment each part of the mass would need to be directly treated with the radiosurgery treatment. It can be difficult for surgeons performing the radiosurgery to isolate each part of the mass.
However; vestibular schwannoma, acoustic neuroma tumor masses from spontaneous tumor growths, not the result of the NF2 condition, would not include more than one mass.
2. Cognitive Thinking (deficiencies in memory and learning): Brain Matter Necrosis
Neurological impairments can develop, based on the area of brain that was treated with radiation and possibly lead to seizures among other problems. ( Department of Nursing, 2011), (Hladik, 2016)
Cognitive Issues:
- Attention
- Auditory Processing
- Working Memory
- Logic and Reasoning
- Long-Term Memory
- Processing Speed
- Visual Processing
- Impaired Mental Status - alertness complications, amnesia, confusion, and disorientation.
- Intellectual Impairment - This is mental retardation due to brain cell death in the area of the brain that was treated.
Rdiation induced necrosis (RIN) is necrosis (cell death) and edema (cell swelling) in the tissues that
surround the area of treatment. While not a tumor, RIN can act like a tumor having mass effects (crowding of other tissues) and may have to be
removed by surgical means. This complication is thought to occur in between 1 and 15% of treatments. (Kim, 2007)
Brain cell death can cause Seizures.
3. Epilepsy and Seizures: Radiation-Induced Necrosis (RIN)
It is not uncommon for epilepsy and seizures to start as a result of radiation treatment on tumors in the skull. When the brain trauma causes epilepsy, seizures will be an ongoing issue for life.
4. More Tumors and Cancer
As a result of the missing or mutated tumor suppressor gene, radiation therapies can place people with NF2, at a higher
risk for growth of additional tumors, increased growth of existing tumors in the surrounding area of treatment and put these patients at
a higher risk of the tumor becoming malignant. While the chance of a tumor becoming malignant is small it is a risk nonetheless. The risk of Cancer
is higher for NF2 patients than non-NF2 patients. [(Wiemels, 2010), (Evans, 2009)]
Highest Risk of Cognitive Issues: Children and Young Adults
At birth and throughout adolescence, the human brain is in a developmental stage. Radiation therapies done before the brain is finished developing leaves people at a higher risk of long-term cognitive issues.
5. Nerve Damage
Radiation can sometimes destroy the nerve the treatment was aiming to save. It can also destroy or damage other nerves as well.
For example sometimes the Facial Nerve is damaged during VS (Vestibular Schwannoma) radiation treatments, but it can also damage the actual
Vestibular Nerve the tumor is growing on. The possible risk of damage to not just the treated nerve but to the surrounding nerves is a reason
that certain areas of the brain cannot be treated with radiation. (Plotkin, 2008)
6. Hearing Implant Damage
A patient with an ABI or CI may have their implant permanently damaged by radiation if it is administered near the device.
The implant should be a specific distance away. The exact distance varies based on radiation doses, but would typically be safe from radiation
treatments on the other side of the brain than the implant.
7. Hair Loss
This might happen only in the area of treatment and may not be permanent. How much hair is lost varies. (Department of Nursing, 2011)
There are specific reasons a form of radiation might make an individual a candidate for a radiation treatment for a specific damaging tumor. Radiation may be more likely to save a nerve or the remaining nerve function that a Schwannoma tumor is growing on, for an extended
period if the treatment is successful. (Lustgarten, 2013) Radiation is worth considering if a tumor is in an inoperable location (too far in the brain to reach), this would not include
tumors close to the brainstem. (Delannes, 2012) The procedure is non-invasive. (Lustgarten, 2013) Radiation might be a better treatment if a patient is not healthy enough to cope with traditional microsurgery. It might be
the only choice in the case where surgery would be life-threatening, elderly patients, very low body
weight patients or patients in general poor health. These patients would not pass pre-surgical screening.
(Husseini, 2013) Recovery from Radiation treatment is short and is often done as an Outpatient procedure. Patients are often released to go
home the same day as the procedure. (UT Dept of Neurology, 2011)) Microsurgery can require a
hospital stay of up to 3 to 15 days. Patient satisfaction is high with radiation treatments. (Lustgarten, 2013) There is a list of factors to discuss with your doctors before having radiation treatment. You should feel comfortable enough with the medical team
you plan to allow to treat you, to ask and make sure they understand your questions and concerns. The list is extensive, and you may only want to discuss some of the questions as others might not apply to your situation. For example, you may not
have an implant. You should ask questions that occur to you that aren't on the list also. Feel free to print the checklist out and take it with
you to your appointments. Take a pen or pencil with you to take notes! Being prepared and knowing what to expect can help reduce anxiety and
stress in children as well as adults. Confirm the doctor is aware that individuals with neurofibromatosis type 2 (NF2) typically have multiple small
schwannomas, not a single mass. These masses can appear as one mass in an MRI. The doctor needs to identify each
part of the schwannoma since the radiation treatment process requires treatment of each part separately. Confirm the doctor is aware radiation treatment can destroy a hearing implant if the treatment is at a high dose close to
the receiver (implanted part of a heating implant). All people are exposed to radiation constantly in our daily lives; this is unavoidable. Radiation is energy that radiates from a source and
travels through space may leave part of its energy in something (matter) it meets. It is capable of stripping electrons from atoms
thereby breaking chemical bonds. It can damage cells and tissues.
However, only Ionizing Radiation is dangerous and can affect the development or growth of tumors. Non-ionizing Radiation energy is too low to
be of much concern. (AFRRI Staff, 2014) Ionizing radiation can cause damage to matter, particularly living tissue. For example, DNA is vulnerable to this type of radiation
and could cause mutations if exposed to enough of it over a long enough period. At a high level, radiation, it is therefore
dangerous, so it is necessary to control our exposure. (World Nuclear News) Sources of the fairly non-damaging non-ionizing radiation include magnetic fields, ultrasound, visible light,
infrared, radio waves, microwaves, power lines, and lasers. There
is still debate among scientists about how non-damaging non-ionizing radiation is.
(Ronca, 2014) Different radiosurgery treatment options for the treatment of inoperable and recurrent benign NF2 tumors are available.
[(Johnson, 2008),(NIDCD, 2010)] During these treatments the head
is; secured in the machine, similar to head hold for brain MRI, and the radiation is set to focus on the tumor. The duration
of treatment the doses is tumor size dependent, specific to the machine, and radiation treatment type. [NIH, 2010]
3. Advantages
1. Potentially Delaying Nerve Damage
2. Inoperable Location
3. Poor Health/Elderly
4. Fast Recovery
5. Patient Refusal of Surgery(Husseini, 2013)
4. Questions to Ask Your Doctor
5. Forms of Radiation
Ionizing Radiation
Non-ionizing Radiation
6. Radiosurgery Delivery Methods
7. Sources
Return to Top of Page
Article: https://www.pnas.org/content/115/9/E2077
http://thejns.org/doi/abs/10.3171/2012.3.JNS111649
https://www.nidcd.nih.gov/health/hearing/pages/acoustic_neuroma.aspx#diagnosed
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2563223/
http://www.nature.com/nrclinonc/journal/v5/n8/full/ncponc1157.html
http://www.ncbi.nlm.nih.gov/pubmed/16222204
http://www.ncbi.nlm.nih.gov/pubmed/23177377
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3654776/
http://www.usuhs.edu/afrri/outreach/ionizing.htm
http://www.nj.gov/dep/rpp/llrw/download/fact03.pdf
http://www.ro-journal.com/content/7/1/210
http://onlinelibrary.wiley.com/doi/10.1002/cncr.26625/full
http://www.sciencedirect.com/science/article/pii/S1278321812000662
http://www.uwhealth.org/healthfacts/B_EXTRANET_HEALTH_INFORMATION-FlexMember-Show_Public_HFFY_1126650982462.html
http://www.sciencedirect.com/science/article/pii/S1383574216300965
http://link.springer.com/article/10.1007/s11060-007-9434-z#page-2
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2739359/
http://www.cancer.gov/cancertopics/factsheet/Therapy/radiation
http://books.google.com/books?hl=en&lr=&id=wVgCSGT_ILoC&oi=fnd&pg=PA103&dq=NF2,+when+to+remove+Schwannoma,+spinal+cord&ots=wwRrfAs-2S&sig=-IrrTfFsIIHp6e3J1R3lxXOl5XI
http://science.howstuffworks.com/radiation2.htm
http://www.ncbi.nlm.nih.gov/pubmed/24529233
http://europepmc.org/abstract/med/27234913
http://neurosurgery.uthscsa.edu/display_patients.php?ps_id=33&pg=patient_services.php.
http://link.springer.com/article/10.1007/s11060-010-0386-3#page-1
http://www.world-nuclear.org/Nuclear-Basics/What-is-radiation-/
https://onlinelibrary.wiley.com/doi/full/10.1002/cam4.266
http://www.ajnr.org/content/early/2015/06/25/ajnr.A4362
https://onlinelibrary.wiley.com/doi/full/10.1002/cam4.266
https://www.cancer.org/treatment/treatments-and-side-effects/treatment-types/radiation/effects-on-different-parts-of-body.html
https://link.springer.com/referenceworkentry/10.1007%2F978-3-319-52619-5_3-1
https://www.sciencedirect.com/science/article/pii/S1878875018325695